The microbiome controls important immune functions in multiple diseases, and there’s a keen interest in using probiotics to manage inflammatory bowel disease (IBD). However, unmodified probiotics don’t treat pathologic inflammation, and previous engineered probiotics have expressed therapeutic proteins in an uncontrolled manner.
Francisco J. Quintana, PhD, a scientist at the Center for Neurologic Diseases at Brigham and Women’s Hospital, Cristina Gutiérrez-Vázquez, PhD, a research fellow at the center, and colleagues have taken a strikingly different approach. They engineered yeasts that generate an immunosuppressive molecule in direct proportion to the amount of a pro-inflammatory metabolite produced in the inflamed gut. In Nature Medicine, they describe their new treatment platform and the results of in vivo murine experiments.
Background
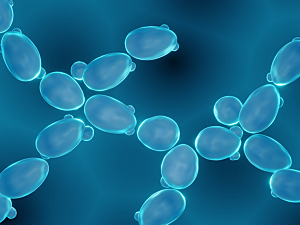
The engineered yeasts are Saccharomyces cerevisiae, a component of the healthy microbiome that’s reduced in patients with IBD. S. cerevisiae has a well-defined signal transduction pathway that can be functionally linked to human G protein–coupled receptors, which enables the controlled expression of proteins in response to disease-associated signals.
One such signal relevant to IBD is extracellular adenosine triphosphate (eATP), which promotes inflammation in the gut. The researchers combined directed evolution and CRISPR–Cas9 gene editing to develop S. cerevisiae probiotics that secrete apyrase in response to eATP. That enzyme depletes eATP and promotes the generation of immunosuppressive adenosine.
Furthermore, the engineered yeasts incorporate a gene circuit that makes them produce different amounts of apyrase depending on how much eATP is present. These self-regulating, highly localized probiotics were designated the “inducible apyrase” strain (indAP).
Mouse Studies
The team tested indAP yeasts against two control strains in a mouse model of colitis:
- indAP yeast administration substantially ameliorated colitis as indicated by evaluation of weight loss, colon shortening and intestinal histology
- The beneficial effects of indAP yeasts were comparable to those achieved by administration of a tumor necrosis factor inhibitor and α4β7 integrin inhibitor similar to those used to treat IBD—drugs that substantially increase the risk of infection and some types of cancer
- Fibrosis can be caused by persistent adenosine signaling, but unlike results with control strains, mice treated with indAP yeasts showed a significant reduction in fibrosis
- Mice treated with indAP yeasts exhibited microbiomes similar to those of mice in which colitis was not induced, suggesting the engineered probiotics may actually re-establish a healthy microbiome
A Generalizable Approach?
eATP promotes intestinal inflammation in diseases besides IBD, including graft-versus-host disease and irradiation-induced abdominal fibrosis. Moreover, the intestinal microbiome controls inflammation at distant body sites such as the central nervous system.
Thus, the methods used to develop these engineered yeasts may lead to self-modulating probiotics for other inflammatory conditions.