As the U.S. health care system turns away from pure fee-for-service care, payers are implementing reimbursement arrangements that incentivize “value,” defined as patient outcomes per dollar necessary to achieve those outcomes. To stay competitive, providers will need to understand costs of the entire cycle of care for the conditions they treat.
Time-driven activity-based costing (TDABC), originally developed for commercial and industrial applications, is being applied to health care because it accounts for all processes and resources used during a patient’s episode of care. TDABC analyses are expected to optimize institutional workflows, inform clinicians’ choices between interventions and support reimbursement negotiations.
George E. Haleblian, MD, urologic surgeon in the Division of Urology at Brigham and Women’s Hospital, and Tyler R. McClintock, MD, formerly of the Brigham, and colleagues applied TDABC to acute urolithiasis, the most costly nonmalignant urologic condition. In Urology, they report wide variation in costs between care pathways, suggesting opportunities to trim inefficient or wasteful services.
Methods
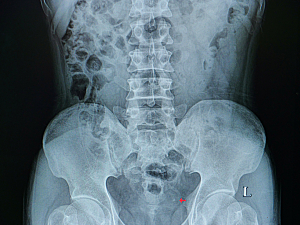
The researchers defined their hypothetical cohort as patients who present to Brigham’s Emergency Department (ED) with any ureteral stone ≤10 mm and have no indication for urgent intervention. Thus, the physician is choosing among medical expulsive therapy, upfront definitive operative intervention and delayed intervention.
The researchers conducted the three steps of TDABC:
1. Map processes—Urologic surgeons created an overarching process map depicting all clinical locations potentially involved in patient care, from initial presentation to the time of being “stone free.” Administrators and clinical supervisors added subprocesses and determined the average amount of time and resource utilization required for each.
2. Determine costs for each resource—Administrators estimated capacity cost rates for personnel, major capital equipment, and clinic space (depreciation-adjusted cost per square foot plus maintenance, operating costs, housekeeping and overhead). Rather than being hospital-specific, salaries and construction costs were based on market rates. Administrators also established the costs of consumable resources.
3. Aggregate costs—The total cost for each step within a subprocess (e.g., draping and preparation for stent removal) was determined by multiplying the cost per minute of staff, equipment, and space by the time required for the process, then combining that figure with the cost of consumables. The cost of all steps was aggregated to determine the total cost for that subprocess—in this case, complete office encounter for stent removal.
Wide Variation in Costs
The team defined eight common clinical pathways for patients who present to the ED:
- Urology clinic, abdominal x-ray plus ultrasound (i.e., successful medical expulsive therapy)—total cost $1,388
- Urology clinic, preoperative center, ureteroscopy with laser lithotripsy (URS), stent removal, ultrasound—$4,353
- Urology clinic, preoperative center, extracorporeal shock wave lithotripsy, ultrasound—$5,311
- URS, stent removal, ultrasound—$5,655
- Percutaneous nephrostomy tube placement, urology clinic, URS, stent removal, ultrasound—$6,574
- Stent placement, urology clinic, URS, stent removal, ultrasound—$7,082
- Repeat ED visit, urology clinic, URS, stent removal, ultrasound—$7,785
- Repeat ED visit, stent placement, urology clinic, URS, stent removal, ultrasound—$8,002
One key takeaway from this list is that temporizing stent placement prior to definitive URS increased costs substantially.
The most expensive individual components of care were URS ($4,057), shock wave lithotripsy ($2,923), stent placement ($1,665), and emergency care ($920).
The Way Forward
Highly accurate, granular data such as this can help organizations better understand and control the costs of high-volume, resource-intensive conditions. When combined with outcomes data, TDABC analyses can help health care systems adjust clinical pathways to focus on value.