Patients living with heart failure (HF) are vulnerable to hospitalization, ICU admission and death if they develop COVID-19. These risks have been demonstrated regardless of ejection fraction and use of renin–angiotensin–aldosterone system (RAAS) inhibitors.
In September 2021, the Heart Failure Society of America published a scientific statement in the Journal of Cardiac Failure that discusses clinical care for patients with HF during the COVID-19 pandemic. Ankeet S. Bhatt, MD, MBA, a clinical and research fellow in the Division of Cardiovascular Medicine at Brigham and Women’s Hospital, served as a co-chair of the writing committee and first author of the document.
COVID-19 and Myocardial Injury
Multiple cases of myocarditis and cardiomyopathy have been reported in patients with COVID-19. However, the term myocarditis has been based on nonuniform criteria including elevation in troponin concentrations, clinical signs of congestion, decrements in ejection fraction, and/or abnormal cardiac MRI findings.
As with other causes of viral myocarditis, it’s unclear whether the cardiac injury results directly from viral infection or is secondary to an unchecked immune response. Complicating matters, it’s becoming accepted that myocardial injury from SARS-CoV-2 may not require myocyte death or an inflammatory cell infiltration.
Myocardial injury in patients with COVID-19 is more common among those with preexisting cardiovascular disease. The degree of myocardial injury and myocardial stretch, evidenced by elevations in cardiac troponin and natriuretic peptide, are strong predictors of poor outcomes.
Acute HF in Patients with COVID-19
New-onset HF related to COVID-19 infection seems infrequent. Still, routine assessment of congestion, including measurement of natriuretic peptides, is important whether or not inpatients with COVID-19 have a history of HF.
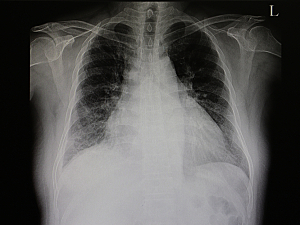
A challenge is an overlap between symptoms and signs of HF and COVID-19, such as shortness of breath and pulmonary infiltrates on imaging. Pleural effusions, cardiomegaly, and inferior vena cava diameter enlargement may signal acute HF and be readily resolved with diuretic therapy.
Management of HF During the Pandemic
Evidence is still accumulating, but current recommendations by drug class are:
- RAAS inhibitors and statins should generally be continued in patients who are at risk for or hospitalized with COVID-19. There is no evidence that discontinuation improves outcomes. Statins may actually benefit hospitalized patients, as randomized trials are examining.
- Anticoagulants—In light of the known prothrombotic state associated with COVID-19, all patients with HF who are hospitalized with COVID-19 should receive prophylactic anticoagulation, and some may benefit from therapeutic anticoagulation. Those with an alternative indication for therapeutic anticoagulation should continue it if there are no contraindications.
- Steroids, immunomodulating therapies (intravenous immunoglobulin) and monoclonal antibodies may require careful monitoring of volume status and additional decongestive therapy in patients with COVID-19 and HF.
- Antiviral agents—No evidence supports a differential approach to their use among patients with HF.
Post-acute COVID-19 Syndrome
Patients can develop post-acute COVID-19 syndrome (PACS, colloquially called “long COVID”) regardless of initial symptom severity. No reports to date suggest a predisposition for PACS among patients with HF, but myopericarditis has been reported six to eight weeks after a COVID-19 diagnosis.
PACS may persist for weeks to months after acute infection, and impaired physical functioning and decreased exercise capacity are common manifestations. Cardiac rehabilitation programs may benefit patients with a history of HF as well as younger patients with de novo cardiac complications.
Vaccination
The CDC recommends booster shots for immunocompromised patients, including those who have undergone heart transplantation. Whether immunosuppression should be altered at the time of vaccine administration is unclear.
The optimal timing and frequency of booster vaccination for non-transplanted patients with HF are also unknown. Isolated cases of myocarditis and HF have been reported after vaccination, particularly in younger adults, but the mechanisms and risk factors are another gap in knowledge.
Other Topics
The detailed scientific statement also addresses:
- Temporary mechanical circulatory support for inpatients with COVID-19 who have HF
- The impact of the COVID-19 pandemic on the care of patients who have undergone or need cardiac transplantation or implantation of left ventricular assist devices
- Telemedicine and implantable devices for remote monitoring
- Racial/ethnic and socioeconomic disparities
- Psychosocial impacts of the pandemic on patients and clinicians
The authors stress that the statement reflects the evidence available at the time of writing and review and is subject to change as new data emerge.