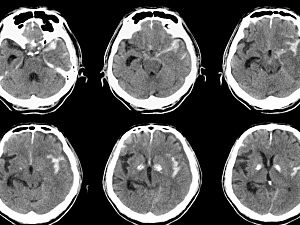
One in four patients with aneurysmal subarachnoid hemorrhage (aSAH) dies before hospital admission. The exact mechanisms of sudden death are unknown, but altered cardiovascular function is a likely culprit. Myocardial injuries occur in about 40% of aSAH cases.
In Neurocritical Care, Christian D. Cerecedo-Lopez, MD, MS, a resident physician, and Rose Du, MD, PhD, director of cerebrovascular surgery in the Department of Neurosurgery at Brigham and Women’s Hospital, and colleagues estimate the U.S. incidence of acute myocardial infarction (AMI) after aSAH is more than 12 times higher than previously reported. They also identify its predictors and quantify its substantial negative effects on outcomes.
Study Cohort
The data source was the National Inpatient Sample (NIS), which provides data on 20% of all discharges from U.S. hospitals. The researchers included 139,734 adults who had aSAH or intracerebral hemorrhage and underwent aneurysm repair between 2002 and 2014.
Incidence of AMI
4,933 patients with aSAH (3.6%) also had diagnostic codes for AMI. By comparison, a previous study of the NIS published in Neurosurgery in 2013 concluded the incidence of AMI after aSAH was 0.28%.
29% of the patients with AMI had ST-elevation myocardial infarction, an incidence of 1.0%.
Predictors of AMI
Independent risk factors for AMI after SAH were:
- Older age—OR, 1.02
- Female sex—OR, 1.18
- Arrhythmia—OR, 1.29
- Pulmonary circulation disorder—OR, 1.43
- Coagulopathy—OR, 1.43
- Poor-grade SAH—OR, 2.84
- Congestive heart failure—OR, 5.37
Protective factors were:
- Aneurysm clipping (vs. coiling)—OR, 0.81
- Uncomplicated hypertension—OR, 0.79
- Complicated hypertension—OR, 0.44
AMI and Outcomes
The primary outcome was poor functional status at discharge, defined as the presence of any of the following: in-hospital mortality, discharge to a skilled nursing facility, extended care facility or hospice, placement of a tracheostomy tube, or placement of a gastrostomy tube.
Compared with patients with aSAH who did not develop AMI, those who did had:
- Higher odds of poor functional status at discharge—OR, 2.9 in the overall cohort; 4.8 in the STEMI subgroup; 2.5 in the non-STEMI subgroup (P<0.001 for each comparison)
- Higher odds of in-hospital mortality—OR, 2.1 overall; 2.9 STEMI; 1.8 non-STEMI (P<0.001)
- Longer hospital stays—mean difference, 4.3 days overall; 4.0 days STEMI; 4.6 days non-STEMI (P<0.001)
- More costly hospitalizations—mean difference, $102,797 overall; $95,774 STEMI; $105,384 non-STEMI (P<0.001)
Besides sudden death, AMI after aSAH can lead to cardiogenic shock, acute pulmonary edema or cardioembolic stroke. Optimizing management is paramount, and distinguishing between STEMI and non-STEMI should be helpful.