The Heart & Vascular Center at Brigham and Women’s Hospital has a well-established reputation for innovation in atrial fibrillation (Afib) treatment. Twenty years ago, the Brigham pioneered cryoablation therapy, which currently comprises about 20 percent of Afib ablations conducted worldwide.
Today, the Brigham takes a comprehensive approach to Afib management, offering a variety of treatments, including surgical ablation, catheter ablation, cardioversion, implantable cardioverter defibrillators, pacemaker implantation and transvenous lead extraction. The Brigham systematically evaluates every patient with Afib and tailors treatments to their specific needs.
“We now recognize that Afib isn’t just one specific cardiac condition,” said Paul C. Zei, MD, PhD, director of the Brigham’s Comprehensive Atrial Fibrillation Program. “There are multiple risk factors, such as obesity, hypertension and diabetes, that affect the likelihood of developing Afib as well as the type of Afib developed.”
Cardiac Ablation Options
According to Dr. Zei, while Afib can be suppressed with anticoagulant and antiarrhythmic medications, ablation is the best strategy to eliminate the rogue electrical signals coming from abnormal cells in the heart.
The Brigham specializes in both surgical and catheter ablation. Surgical ablation — whether through median sternotomy or thoracotomy — allows surgeons to visualize the entire heart and treat wider swaths for more thorough treatment. However, as with any invasive surgery, it carries a higher risk of morbidity and requires longer recuperation.
Dr. Zei added that data on surgical outcomes is limited, with few prospective and large patient population studies. “We don’t have a good way to evaluate the electrical outcomes of surgery and make sure that the desired electrical blockages have occurred,” he said.
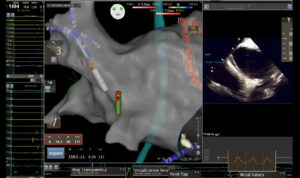
Catheter ablation, on the other hand, is a less invasive procedure and delivers precise energy to heat or freeze, and thus destroy, the areas causing the abnormal heart rhythm. However, because it is so precise, catheter ablation is limited in its ability to target wide swaths, leaving some tissue untreated.
“Catheter ablation requires a tremendous amount of training and skill,” Dr. Zei said. “Here at the Brigham, we perform hundreds of these procedures every year with excellent outcomes.”
Combining Advantages of Surgical and Catheter Ablation
Traditional ablation techniques have been used successfully for several decades. According to Dr. Zei, however, the prevalence of Afib in the population and the condition’s high cost have prompted the cardiac care community to improve how it performs the procedure and the technologies used to do so.
One new technology used by the Brigham is a minimally-invasive epicardial/endocardial ablation known as hybrid convergent. This new approach provides superior effectiveness compared with traditional catheter ablation for persistent and long-standing Afib.
While the procedure is new and data on effectiveness continues to develop, Dr. Zei said some of the Brigham’s patients are already taking advantage of it.
“The procedure is ideal for patients for whom a single catheter procedure is not likely to be successful,” he said. “That includes patients who have advanced Afib that has persisted for several years. Those patients tend to have enlarged atria with significant abnormal electrical activity that can’t be covered completely by catheterization.”
New Interventions to Improve Patient Outcomes
In addition to clinical patient management, Dr. Zei and his colleagues are leveraging the Brigham’s vast patient population to conduct research on how various interventions, from ablation and surgery to risk factor modifications and genetics, affect patient outcomes. Dr. Zei also is pioneering new approaches to treating Afib, including using noninvasive external beam radiation to treat arrythmias and an ablation procedure that eliminates the need for fluoroscopy.
“We have a robust program of basic science and clinical research within the Brigham’s Heart and Vascular Center,” he said. “This program has generated promising results for improving cardiac care for arrhythmias.”
Full image caption: This image depicts the operator’s typical viewpoint during catheter ablation for atrial fibrillation. The central image left-of-center shows an electroanatomic (EA) shell map of the left atrium, as viewed from an anterior projection. The ablation catheter (white cylinder with green/red tip, and mapping catheters (blue multi-splined catheter and green intracardiac echocardiography (ICE) ultrasound tip) are also projected onto the map. The right-of-center image shows a simultaneous intracardiac ultrasound (ICE) view of the left atrium from the ICE catheter. These detailed, accurate renderings help guide the operator during ablation, without use of fluoroscopy, enabling a safe, effective, and efficient ablation procedure.