The once-long road to developing a viable alternative to kidney dialysis has become a little shorter thanks to strides made by a unique public-private partnership.
The Kidney Health Initiative—established in 2016 by the American Society of Nephrology and the U.S. Food and Drug Administration—has made significant progress in developing a Technology Roadmap. This document identifies design criteria to replace the myriad functions of the kidney in a manner that will replace traditional dialysis as we know it and improve the lives of individuals with renal disease.
Joseph V. Bonventre, MD, PhD, chief of the Division of Renal Medicine at Brigham and Women’s Hospital, was co-leader and one of the roadmap’s principal architects. He continues to drive the partnership’s push to reduce the morbidity and mortality rates associated with end-stage kidney disease.
“The Technology Roadmap is a living document,” he said. “It outlines the scientific, technical, regulatory and payor milestones required to commercialize and provide patient access to a range of kidney replacement therapy alternatives.”
‘A Renewed Sense of Urgency’
Dr. Bonventre pointed to a number of positive developments in the past year, including President Trump’s signing of the Advancing American Kidney Health initiative in July 2019. The initiative is designed to reduce the number of people developing kidney failure, reduce the number of people receiving dialysis in dialysis centers and make more kidneys available for transplant.
“That executive order built on the original roadmap and really spurred a renewed sense of urgency that has helped the community come together around nephrology innovation at a number of levels,” Dr. Bonventre said.
One track of innovation involves the development of home therapies, including an artificial “wearable” kidney and smaller, user-friendly dialysis machines.
“The Center for Medicare and Medicaid Innovation is responding by forming new health care payment models that will reduce costs by encouraging home therapies,” Dr. Bonventre explained. “We’re also seeing support from Health and Human Services in general, as well as the National Institutes of Health.”
Another track of innovation focuses on the potential of xenotransplantation using pig kidneys. Dr. Bonventre touted significant breakthroughs that have been made in eliminating the pig viruses that have previously raised concerns and reduced enthusiasm for this approach to treatment.
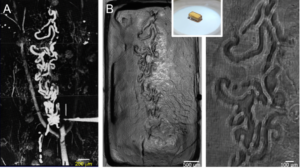
Dr. Bonventre said the community also continues to expand its basic research to identify new therapeutic agents that can prevent chronic kidney disease, kidney injury and kidney fibrosis. One example in development is the creation of “mini kidneys” made from stem cells, which his laboratory pioneered.
“It’s exciting to see engineering firms, biopharmaceutical companies and even smaller startups launching new programs in areas they weren’t participating in before,” he said. “People everywhere—from the public to pharma, venture capital and the government—are now talking about the kidney and opportunities to bring new therapies to patients with kidney diseases in whole new ways.”
On the Front Line of Innovation
In addition to Dr. Bonventre’s work in helping to bring innovation to prevention and treatment of chronic and advanced kidney disease, teams of physicians, researchers, materials scientists and biomedical engineers at the Brigham and its sister institutions are working diligently toward solutions. Dr. Bonventre is also collaborating with a team established by the U.S. Department of Defense to create a wearable kidney support device that will complement a pulmonary support system for injured soldiers.
As another example of Renal Division leadership in innovation for kidney patients, Dirk M. Hentschel, MD, director of interventional nephrology at the Brigham, is collaborating with the medical technology company Humacyte® to develop an “off-the-shelf” human blood vessel for dialysis access. Additional projects in the division are focusing on immunosuppression and identification of biomarkers to help predict which patients with kidney disease will develop worsening kidney function.
“These are just a few of the latest kidney disease research and treatment programs from the institution that partnered with Willem Kolff, the ‘Father of Artificial Organs,’ to develop the Kolff-Brigham artificial kidney, created commercial dialysis, conducted the first kidney transplant and gave us the ability to make kidney cells out of stem cells—breakthroughs that have improved the lives of countless patients over the years,” Dr. Bonventre said.