A soon-to-be published study reports a high prevalence of interstitial lung abnormalities (ILA) and undiagnosed interstitial lung disease (ILD) among first-degree relatives of patients with familial pulmonary fibrosis (FPF) and sporadic idiopathic pulmonary fibrosis (IPF). Results suggest screening might be warranted for undiagnosed relatives to facilitate early detection of PF.
Gary M. Hunninghake, MD, is the first and corresponding author of the study, a collaboration with Benjamin Raby MD, MPH, chief of the Division of Pulmonary Medicine at Boston Children’s Hospital, and Ivan Rosas, MD, chief of the Division of Pulmonary, Critical Care and Sleep Medicine at Baylor College of Medicine. Their paper has been accepted for publication by the American Journal of Respiratory and Critical Care Medicine.
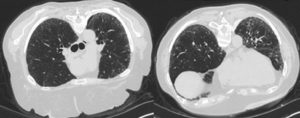
Dr. Hunninghake, director of the Interstitial Lung Disease Clinic and Sarcoidosis Service at Brigham and Women’s Hospital, has focused on identifying early stages of PF for a decade. “We’ve published a number of papers demonstrating there are people who have early changes on their CT scan but don’t yet know they have ILD,” he said. “These people tend to have many of the same physiologic abnormalities we would expect in people with ILD, although often in a less severe form.”
More recently, Dr. Hunninghake and colleagues have published several papers highlighting a genetic overlap between these undiagnosed individuals who have imaging abnormalities and patients with IPF. These findings, in turn, have raised many significant questions. For example, might screening help to identify people in their earliest stages of the disease? And should there be a sharp distinction between FPF (when multiple members of a family have IPF) and IPF (when only one family member is affected)?
“Sporadic IPF is felt to be the most common form of the disease and to comprise isolated cases,” Dr. Hunninghake said. “For this study, we operated under the premise that this might not be true—that there might be an increased risk of early changes in both families and in individuals with sporadic disease.”
A Surprisingly High Rate of Interstitial Changes
Undiagnosed first-degree relatives of patients with PF were invited to take part in the study. All participants underwent comprehensive evaluations (the results of which were kept as protected health information), and physicians and genetic counselors followed up with them to explain the results.
Among the key findings: Thirty-three (31 percent) of the 105 participants had ILA on CT, while the remainder were either indeterminate or had no ILA. Of those with ILA, 19 (58 percent) had further evidence for ILD.
The investigators were surprised by the rate of interstitial changes in participants. “Even if you limited the important cases to those who had either more advanced fibrotic imaging findings alone or less-advanced imaging evidence of fibrosis, but significant reductions in either lung volumes or gas exchanges, 18 percent of the people we screened were abnormal,” Dr. Hunninghake said. “That’s a strikingly high rate for a screening study in general.”
Eradicating an Arbitrary Distinction?
Investigators also found that one in six older first-degree relatives of patients with PF may have an undiagnosed form of ILD—and that there was no statistical difference in the rates of imaging changes between participants associated with FPF as opposed to with sporadic IPF.
“I think this latter point will be critical in the future because it suggests this distinction we’re making is likely arbitrary,” he said. “In addition, we might have to seriously consider there is an elevated risk of at least an early stage of PF that’s common to families regardless of whether there’s only one or multiple cases known in the family.”
Dr. Hunninghake added that screening of relatives eventually could become an effective method for identifying people with undiagnosed PF. “We hope, and our data supports the idea, that future studies may demonstrate ways we can intervene to prevent these people from getting more advanced stages of disease,” he said.
Finally, the study findings showed that pulmonary function testing, telomere length assessments and some element of genetic screening may be helpful in risk-stratifying relatives for undiagnosed ILA.
“That’s something we think would be important to follow up on and verify,” Dr. Hunninghake concluded.