Increased immune system activity at the brain’s surface, or meningeal inflammation, is believed to be important for understanding how relapsing remitting multiple sclerosis (RRMS) — the most common early form of the disease — progresses to more advanced clinical stages. But the most commonly available MRI technology, 3 Tesla (3T), offers a limited view of meningeal inflammation.
Recent research by Jonathan Zurawski, MD and colleagues in the Department of Neurology at Brigham and Women’s hospital provides new insight into the potential role for leptomeningeal enhancement (LME), or contrast enhancement, on the surface brain visualized with specialized post-contrast MRI techniques as a marker of MS severity. Using Brigham and Women’s powerful 7 Tesla (7T) MRI — the second in the United States to be approved for clinical use — the investigators found that this proposed marker of brain inflammation in MS patients is more common (seen in two-thirds of patients) than previously reported and is tied to lesions in the gray matter regions of the brain. The team’s findings are published in the Multiple Sclerosis Journal.
“The 7T MRI scanner is capturing a more nuanced view of the brain, specifically looking at the gray matter structures and the leptomeninges, which are not seen very well with conventional [3T] MRI,” said Zurawski, the study’s corresponding author. “The 7T scanner reveals markers or signatures that were poorly characterized or overlooked and may allow us to better understand the disease process and ultimately better treat MS patients.”
Zurawski and his co-authors work within the Partners Multiple Sclerosis Center at Brigham and Women’s Hospital, where physicians care for and follow disease progression in nearly 3,000 MS patients yearly. The Center is one of the largest in the country for MS clinical care.
LME Found in Two-thirds of RRMS Patients, Who Also Show Increased Gray Matter Injury
To conduct their study, the team enrolled 30 participants with RRMS and 15 heathy control subjects. All participants underwent detailed 7T MRI scans to look for signs of LME and gray matter lesions.
The team found that 20 out of 30 (67 percent) of MS subjects had LME compared to only one of the 15 healthy people (6.7 percent), a tenfold increase. (Previous studies of MS patients using 3T MRI found LME in approximately 25-50 percent of subjects.) MS patients with LME also had a four-to-five-fold increase in cortical and thalamic lesions, telltale signs of gray matter injury seen in MS. LME was more strongly linked to gray matter than white matter lesions, the traditional measure of MS by MRI.
The authors concluded that LME is common in RRMS at 7T and hypothesized that “cerebrospinal fluid (CSF)-related inflammation links cortical and thalamic injury.” They suggested that in addition to white matter inflammation, which is classically believed to underlie MS, a complimentary process involving inflammatory factors in the CSF may be important in driving gray matter injury adjacent to the ventricles and at the brain’s surface.
One difficulty with MS is understanding how and whether white matter changes that traditionally have characterized the early disease are related to gray matter injury that seems to accumulate as the disease progresses.
“Our job as clinicians is to try to better understand how the two processes are related and to monitor them both as best we can. The 7-T MRI may open the window to monitoring that second process that may be going on,” Zurawski said. “Gray matter injury is an important part of MS, which may be a key factor driving disease progression. Our hope is that by finding new markers of this progression, it opens the opportunity for developing treatments that can prevent progression before lesions become widespread. And, following the extent of gray matter injury in the brain may give us a better sense of how well therapies are working.”
Although study was limited by its small sample size, the research team is expanding the study’s size to include more patients in the future. And plans are underway to continue following the patients in this study over time to see how LME and gray matter lesions may change over months and years and in response to treatment. Future research may include looking at whether subtle symptoms or signs of clinical worsening correlate to changes in gray matter and LME.
Expanded Uses of State-of-the-Art 7T MRI
A 7 Tesla MRI group meets regularly at the hospital — including neurologists, radiologists, neurosurgeons, MRI technologists and MRI physicists— to address ongoing and new uses of the technology.
“The 7T is a very exciting new tool for potential collaboration in neurology and neurosurgery – and beyond the brain and into orthopedics and other fields of study,” Zurawski added. “The 7T MRI has the potential to provide new insight into many different disease processes that will hopefully translate to new clinical advances that benefit patients.”
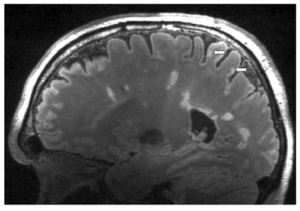
*This 7 Tesla image from a multiple sclerosis patient scanned on the Brigham & Women’s Hospital 7T Siemens Magnetom MRI shows representative periventricular white matter lesions traditionally seen in MS as well as two cortical lesions (white arrows) that are better visualized with 7T MRI.
As seen in Multiple Sclerosis Journal, https://journals.sagepub.com/doi/pdf/10.1177/1352458519885106