Researchers at Brigham and Women’s Hospital have identified several links between the use of immune checkpoint inhibitors (ICPIs) and acute kidney injury (AKI). The risk factors, clinicopathologic features, treatment and long-term outcomes in patients with ICPI-associated AKI, as well as the risk of recurrent AKI with ICPI rechallenge, are detailed in a multicenter study recently published in the Journal of the American Society of Nephrology. These newly identified links will help guide oncologists in treating patients with ICPIs.
“Immune checkpoint inhibitors have revolutionized oncology,” said the study’s senior author, David E. Leaf, MD, MMSc, FASN, associate physician in the Brigham’s Division of Renal Medicine. “While they are now a first-line treatment for a range of malignancies, as they have been shown to prolong progression-free and overall survival, they can also cause a unique spectrum of autoimmune toxicities known as immune-related adverse events.
“These autoimmune side effects can affect virtually any organ, including the skin, GI tract, endocrine system and kidneys. As the use of these agents continues to expand, it is likely that nephrologists will be increasingly charged with diagnosing and managing AKI caused by these medications.”
Prior Study of ICPI-AKI
Dr. Leaf’s lab has been studying the link between ICPIs and AKI for over five years and published the first multicenter case series on the subject in 2016 in Kidney International. At the time, ICPIs were relatively new and there were only a few isolated case reports describing an association with AKI.
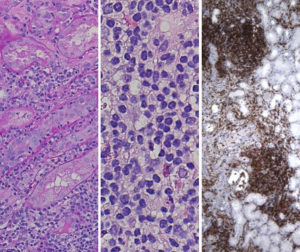
With the goal of learning more about the science, Dr. Leaf reached out to oncologists, nephrologists and pathologists around the country and identified 13 patients with kidney biopsy-proven ICPI-AKI. The investigation found that 12 of the patients had acute tubulointerstitial nephritis (AIN) and that the clinical features of ICPI-induced AIN mirror other etiologies of AIN. (Patients often present with pyuria and sub-nephrotic range proteinuria, and most patients respond to steroids.)
“While this first investigation helped us start to define the clinical features, pathology and response to treatment in patients with ICPI-AKI, the number of patients studied was relatively small,” Dr. Leaf said. “I therefore wanted to conduct a much larger follow-up study to identify risk factors for development of ICPI-AKI and to determine the safety of rechallenging patients with an ICPI following an episode of AKI, a treatment decision that carries enormous weight.”
Current Multicenter Study the Most Comprehensive to Date
For the current multicenter study, Dr. Leaf led the effort to identify 138 patients with ICPI-AKI from 18 institutions across the United States and Canada. Patients were included if they had AKI attributed to an ICPI by their treating provider(s). Only patients with moderate-to-severe AKI (defined as either a >two-fold increase in serum creatinine or the requirement for dialysis) were included. The team also collected data on 276 contemporaneous control patients who received ICPIs but did not develop AKI.
The study’s goals were to determine:
- The independent risk factors for development of ICPI-AKI
- The clinical and pathological features associated with ICPI-AKI
- The key factors associated with renal recovery following an episode of ICPI-AKI
- The risk of recurrent AKI with ICPI rechallenge
- The impact of ICPI-AKI on overall survival
Compared to controls, patients with ICPI-AKI had a lower pre-treatment median estimated glomerular filtration rate. They were also more likely to be receiving combination ICPI therapy and to be receiving therapy with a proton pump inhibitor. Complete, partial and no renal recovery occurred in 40 percent, 45 percent and 15 percent of patients, respectively. ICPI rechallenge occurred in 22 percent of patients, of whom only 23 percent developed recurrent ICPI-AKI.
“This study identifies patients who should likely be monitored more closely for AKI following initiation of treatment with ICPIs. Further, the study findings should encourage oncologists to strongly consider ICPI rechallenge following an episode of ICPI-AKI that has resolved/stabilized, especially if the patient lacks other viable treatment options,” Dr. Leaf concluded. “With support from my colleagues at the Brigham, I am planning a follow-up study examining ICPI rechallenge in more detail. I will also be studying whether biomarkers in the blood or urine can be used to diagnose ICPI-AKI noninvasively and to better understand its pathophysiology.”