The NuPulseCV Intravascular Ventricular Assist system (iVAS) is a novel, minimally invasive mechanical circulatory support device that provides long-term support for patients with advanced heart failure who are not benefiting from medications or cardiac resynchronization therapy.
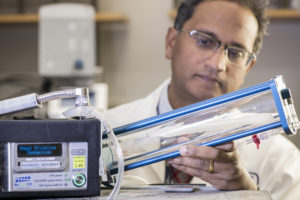
A balloon-like mechanical device, iVAS is placed in the descending aorta and supports failing circulation as a bridge-to-transplant, bridge-to-recovery or bridge-to-decision (transplant or left ventricular assist device). Unlike previous mechanical circulatory support devices, iVAS does not require a large incision through the chest.
The results of the first-in-human trial of iVAS were published in a 2019 issue of Journal of Heart and Lung Transplantation. The trial enrolled 14 bridge-to-transplant patients and 13 were implanted with the iVAS device. Twelve of the 13 iVAS-implanted patients survived to transplant or experienced stroke-free survival at 30 days.
The Brigham is the first center in New England to investigate iVAS
In 2019, the Heart & Vascular Center at Brigham and Women’s Hospital became the first center in New England to participate in a multicenter feasibility study to evaluate whether iVAS can support patients with advanced heart failure for up to several months at home. The study aims to enroll about 100 patients with 10 patients likely to receive implantation. The trial could lead to FDA approval for commercialization in 2021.
“We are excited to be the first center in New England to adopt the iVAS system, which may offer advantages to patients who are either waiting for heart transplantation or not yet eligible for transplantation. We were chosen as a site, because the Brigham has an outstanding track record of leadership in investigating novel device therapies for advanced heart failure,” says Michael M. Givertz, MD, medical director of Heart Transplant and Mechanical Circulatory Support at the Brigham.
The Brigham’s Heart & Vascular Center has pioneered the examination of many mechanical circulatory support devices, including the recently approved HeartMate 3, whose pivotal MOMENTUM trial was led by Mandeep R. Mehra, MD, the executive director of the Center for Advanced Heart Disease at the Brigham.
iVAS is first major advance in the intra-aortic balloon pump in 50 years
“We knew we had to get access to this new technology, so we could offer it to our patients. iVAS is the first dischargeable intra-aortic balloon pump—really the first major advance in the intra-aortic balloon pump in 50 years,” says Hari Reddy Mallidi, MD, executive director for ECMO at the Heart & Vascular Center and surgical director of Heart Transplant and Mechanical Circulatory Support at the Brigham.
iVAS is controlled by a small drive unit contained in a satchel that can be worn over the shoulder. The implanted device communicates with an external drive unit via placement of electrodes under the skin and a skin interface device. Most patients can walk the day after surgery and are ready to be discharged home following a short recovery.
Since iVAS allows patients mobility, they can wait for their heart transplant at home versus staying in the hospital. Patients can also participate in rehabilitation to get into better physical condition before transplantation.
“iVAS allows physicians to discharge patients with heart failure support, short of a fully implantable LVAD,” says Dr. Mallidi. “It also allows us to intervene on patients at an earlier stage in heart failure and potentially delay the progression of their condition.”
Two patients have received an iVAS at the Brigham’s Heart & Vascular Center
To date, the Heart & Vascular Center has implanted iVAS in two patients with advanced heart failure. The first patient had failed standard medical therapy and was not a candidate for a traditional left ventricular assist device.
“This patient received an iVAS and underwent a successful heart transplant. He’s extremely grateful for his new heart and expects an excellent quality of life. The most recent iVAS-implanted patient is home, waiting for transplantation,” says Dr. Givertz.
The iVAS device has been easy for patients to manage at home. It’s more comfortable and less cumbersome than older intra-aortic balloon pumps, and patients seem to get used to the machine’s pulsing sound, according to Dr. Mallidi.
Implantation involves a multidisciplinary team of advanced heart failure experts
The iVAS implantation surgery involves collaboration between multiple teams within the Heart & Vascular Center, including interventional cardiology, advanced heart failure, cardiac surgery and critical care cardiology. Colleagues in cardiac imaging also help decide whether patients are appropriately sized for iVAS.
“As with the adoption of any advanced therapy for heart failure, success depends on having a well-functioning, multidisciplinary team. This is another way Brigham is a leader in cardiac care, particularly in advanced heart failure,” says Dr. Mallidi.
David A. Morrow, MD, MPH, director of the Levine Cardiac Intensive Care Unit (LCU), leads the care of patients before they transition to the step-down unit.
“With temporary mechanical support, we always want our patients to remain awake, mobile and participatory in their care. We are very pleased to be investigating this new device that may allow us to achieve these goals,” says Dr. Morrow.
After iVAS-implanted patients leave the LCU, a combined medical surgical unit provides day-to-day care, helping them transition from short-term rehabilitation to their home.
“The Brigham has played key roles in the evolution of advanced care for heart failure. Our adoption of iVAS demonstrates how we are continually at the leading edge of investigating novel technologies for end-stage heart failure,” says Dr. Mallidi.