 A study presented at the 2019 ASCO Annual Meeting showed that radiation therapy prior to surgery does not reduce the rate of local recurrence among most patients with retroperitoneal sarcoma (RPS). Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC) was the only U.S. center to participate in the European trial of 256 patients.
A study presented at the 2019 ASCO Annual Meeting showed that radiation therapy prior to surgery does not reduce the rate of local recurrence among most patients with retroperitoneal sarcoma (RPS). Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC) was the only U.S. center to participate in the European trial of 256 patients.
“Until now, expert sarcoma centers have been following inconsistent treatment plans for RPS,” said Chandrajit Raut, MD, MSc, surgery director, Center for Sarcoma and Bone Oncology at DF/BWCC. “Some believed there was a benefit, while others did not, and when radiation was used, it was often delivered using different doses and modalities.”
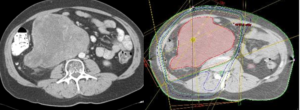
Dr. Raut served as lead investigator of the study along with Elizabeth Baldini, MD, MPH, director of sarcoma radiation oncology at DF/BWCC. He explained that one of the reasons radiation therapy had been used for RPS patients was its success in reducing recurrence in patients with sarcomas in the arms and legs. However, those sarcomas tend to be smaller and more easily resected compared to RPS, which accounts for about 15 percent of all sarcomas.
“Due to their location in the abdomen, RPS can grow quite large before patients feel symptoms, or they are discovered on scans obtained for other reasons,” he said. “Because of their large size as well as the difficulties of surgically removing them with wide negative margins, recurrence rates are higher, and prognosis is worse than for sarcomas of other sites. Liposarcomas, which represent about two-thirds of all sarcomas in the retroperitoneum, have a particularly high risk of local recurrence, while leiomyosarcomas in the retroperitoneum have a high risk of spreading elsewhere in the body.”
Although the overall trial was negative, according to Dr. Baldini, this “practice-changing” study suggested a benefit to conducting radiation before surgery for a small subset of liposarcoma patients.
“Unlike the trial patients who had leiomyosarcoma, those with well-differentiated liposarcoma appeared to benefit from radiation,” she said. “Because of this, we still consider radiation on a very individualized basis.”
Dr. Raut said now that a new standard has been set for treating RPS with respect to radiation, he is turning his attention to studying the effect of pre-operative chemotherapy for certain subsets of RPS patients.
“The radiation study helped to define future trials for RPS treatments,” he said. “It was also a wonderful example of how DF/BWCC can collaborate internationally to answer questions about a rare disease through carefully coordinated efforts.”
Dr. Raut noted that although DF/BWCC is one of the world’s busiest sarcoma centers, enrolling patients in RPS trials can be challenging because many Americans are treated in local clinics before they get an opportunity to be referred to a trial center.
“Patients in Europe tend to benefit from better centralization of rare-disease care,” he added. “Here in the United States, many patients initially get treated at their local institutions, where there may not be clinicians with sarcoma expertise. Fortunately, many patients come from throughout the U.S. and from other countries to participate in sarcoma trials and care at DF/BWCC, where we integrate care among all disciplines with unparalleled expertise across radiation, surgery, medical oncology and pathology.
“We’re committed to maintaining our position as an international leader in this field and to developing new trial designs and novel treatments that will push the boundaries of care and solve unmet patient needs.”